How to Prevent Postural Complications in Wheelchair Users: Strategies for Occupational Therapists
Postural complications can impact wheelchair users’ independence and comfort. Explore strategies to assess, prevent, and address these challenges effectively.
February 3, 2025
8 min. read

Identifying, achieving, and maintaining an optimal seated position provides postural alignment, mitigates pressure risk, enhances function, and provides comfort for wheelchair users. Each client is unique and may present with decreased range of motion, orthopedic changes, abnormal muscle tone, muscle weakness or paralysis, and other issues. These issues make achieving optimal posture a nuanced process, requiring a comprehensive mat assessment to identify challenges and develop practical, tailored solutions.
As occupational therapists, we understand that an optimal position and seating system solution is never one-size-fits-all. Every client brings unique challenges, and their differences require a thoughtful, personalized approach to create recommendations that prioritize comfort and function, empowering clients to engage in meaningful daily activities.
My goal is to equip OTs with practical insights for improving clients’ quality of life through individualized wheelchair seating assessment and intervention. In this article, we’ll explore foundational strategies for addressing postural challenges, identify solutions, and dive into real-world case studies that demonstrate how tailored interventions can lead to meaningful outcomes.
Understanding postural complications
Suboptimal positioning in wheelchair users often hinders their ability to engage fully in daily life. These challenges may develop subtly but have far-reaching impacts on independence, comfort, and health. By recognizing these issues early and implementing strategic interventions, we can prevent secondary complications and enhance our client’s participation in meaningful activities.
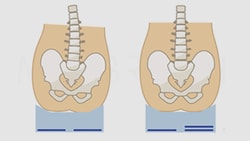
Pelvic positioning issues
Pelvic positioning is foundational to overall posture, as it directly impacts spinal alignment, pressure risk, comfort, and functional engagement in daily activities. Asymmetries such as posterior pelvic tilt, anterior pelvic tilt, rotation, or obliquities often lead to secondary complications, including spinal curvatures, increased pressure risk, impaired function, and discomfort. These issues can stem from abnormal muscle tone, range of motion limitations, habitual postures, or improperly configured seating systems.
A thorough mat assessment determines whether pelvic issues are flexible (reducible) or fixed (non-reducible), which guides decisions about correction or accommodation in the wheelchair seating system. Early intervention in pelvic alignment can help prevent the progression of related postural asymmetries.
Scoliosis and lateral asymmetries
Lateral spinal curvature, or scoliosis, kyphosis, and lordosis are common issues for wheelchair users. Without proper intervention, spinal curvatures can progress, causing discomfort, reduced function, and increased risk of pressure injuries.
Early detection is critical. During the mat assessment, we can identify whether spinal curvatures are reducible or non-reducible, shaping the type and level of support needed. For some clients, specific seating systems can slow progression and improve alignment, even when complete correction isn’t possible.
Muscle tone-related challenges
Muscle tone plays a significant role in posture. Increased tone can pull the body into undesirable positions, leading to asymmetries if not addressed. Conversely, low tone often results in a collapsed posture, as the body struggles to resist gravity.
For clients with increased tone, strategies including selecting optimal seated angles, using inhibition techniques, providing movement, and promoting functional positioning are effective. For those with low tone, external support systems, including molded seating or tilt-in-space features, can provide the stability needed for the client to find optimal posture support to engage in meaningful activities.
4 strategies for preventing postural complications
Conduct comprehensive assessment, including the mat assessment, to identify individual seating challenges
Match client parameters to appropriate seating solutions
Reevaluate, as needed
Integrate sleep positioning strategies
Preventing postural complications in wheelchair users demands a strategic approach. Comprehensive evaluations, individualized solutions, and regular adjustments allow us to make a lasting impact on our clients’ posture, function, and quality of life. Let’s take a closer look at four key strategies that form the foundation of effective postural management:
1. Conduct comprehensive assessments
A thorough mat assessment is critical. Evaluating muscle tone, range of motion, and postural tendencies provides invaluable insight into the client’s needs. This evaluation lays the groundwork for designing a seating system that aligns with their physical abilities and goals while addressing potential complications before they arise.
2. Match client parameters to appropriate seating solutions
A wide range of seating systems are available, from off-the-shelf solutions to molded seating systems. These customized solutions enable improved alignment, stability, and function and reduce pressure risk, ensuring the seating system supports—not restricts—the client’s goals.
3. Reevaluate, as needed
Postural needs can change over time due to growth, change of condition, or medical interventions. Regular follow-ups allow occupational and physical therapists to reassess the seating system’s effectiveness and make adjustments or further recommendations to maintain optimal support over time.
4. Integrate sleep positioning strategies
Posture doesn’t start and stop with the wheelchair. It is important to assess all the positions a client is in within a 24-hour time period, including the wheelchair, other adaptive seating, standers, etc. Nighttime positioning is critical to 24-7 postural care management, as lying posture influences sitting alignment the following day. Studies show that it promotes body alignment, reducing the risk of asymmetries.1
Case studies: Addressing tone, range of motion, posture, and alignment challenges
Postural challenges reveal the complex interplay between muscle tone, range of motion, postural alignment, and functional limitations. Let’s explore two cases demonstrating how thoughtful, targeted interventions can create transformative outcomes.
Taylor: Managing high tone and extension
Taylor, an eight-year-old with cerebral palsy, presented with significant extensor tone that made maintaining an optimal seated posture difficult. His strong extension pushed him into a posterior pelvic tilt, and imbalances of muscle tone in the trunk led to lateral trunk flexion, compounding his postural asymmetries and creating a challenge for functional positioning.
Mat assessment findings
The mat assessment determined Taylor’s available range of motion and his pronounced tendency toward extension. This insight highlighted the need for specific support angles to inhibit tone and promote a neutral alignment to accommodate his physical needs without increasing the risk of further postural issues.
Intervention
A molded seating system was designed to fit Taylor’s body in the identified posture and inhibit the intense forces created by his extensor tone by increasing pressure distribution. The seating system provided intimate contact and stability while ensuring his body’s alignment and respecting his available range of motion.
Outcomes
The customized seating system allowed Taylor to achieve improved posture and head control. This alignment enabled him to use his communication device effectively, significantly enhancing his participation in school activities and social interactions.
Key takeaways
Addressing tone-related challenges requires a combination of specific seated angles and supportive surfaces to stabilize posture and prevent loss of range and asymmetries. Proper assessment and intervention can enable clients like Taylor to reach functional goals that were previously out of reach.
Riley: Low tone and collapsing posture
Riley, a three-year-old with developmental delays, exhibited different challenges. Her low tone resulted in a collapsing posture, characterized by reducible kyphosis and lateral scoliosis. Because her body lacked intrinsic stability, gravity and habitual postures further exacerbated her asymmetries, making intervention essential to prevent further deterioration.
Mat assessment findings
Riley’s assessment highlighted her hypermobility and a tendency toward right lateral trunk flexion, particularly during sleep. Her pelvis also showed signs of rotation and obliquity, which significantly influenced her spine’s alignment and postural control.
Intervention
A molded seating system was designed to provide comprehensive support for Riley’s trunk and pelvis. In combination with the tilt-in-space manual wheelchair, it helped to counteract gravity’s effects, redistribute pressure, and promote an upright posture, enhancing her stability and engagement.
Outcomes
This intervention successfully improved Riley’s pelvis and trunk alignment, enabling her to engage in communication activities more effectively and maintain a stable posture for play and interaction with her environment.
Key takeaways
Managing low tone in wheelchair users requires prioritizing pressure distribution and external support to replace the stability the client lacks internally. Incorporating tilt-in-space features and comprehensive trunk and pelvic support can mitigate gravitational forces, enhance alignment, and ultimately improve the client’s ability to engage in meaningful activities.
Transforming lives through better positioning
Effective wheelchair positioning goes beyond achieving appropriate posture—it supports independence, comfort, and meaningful participation in daily life. By focusing on individualized strategies, from thorough assessments to customized solutions and monitoring, we can address the unique challenges our clients face while fostering greater quality of life.
As Taylor and Riley’s cases demonstrate, thoughtful, customized interventions can create transformative outcomes, even for the most complex postural needs. Applying these principles can help clients overcome barriers, achieve their goals, and engage more fully in the activities that matter most to them.
Do you feel equipped to tackle the complexities of wheelchair positioning? If you’re ready to expand your skills, check out my Medbridge courses for expert insights, practical techniques, and real-world strategies to elevate your clinical practice:
References
Osborne LJ, Gowran RJ, Casey J. Evidence for 24-hour posture management: A scoping review. British Journal of Occupational Therapy. 2023;86(3):176-187. doi: 10.1177/03080226221148414
Below, watch Michelle Lange discuss a case study in this brief clip from her Medbridge course "Wheelchair Positioning: Tying It All Together—A Series of Case Studies."